Conference starts in -973 days


Keynote speakers
Introducing our esteemed keynote speakers, poised to enrich the ACPE2025 conference program with their unparalleled insights and expertise.
More speakers will be announced over the coming weeks.
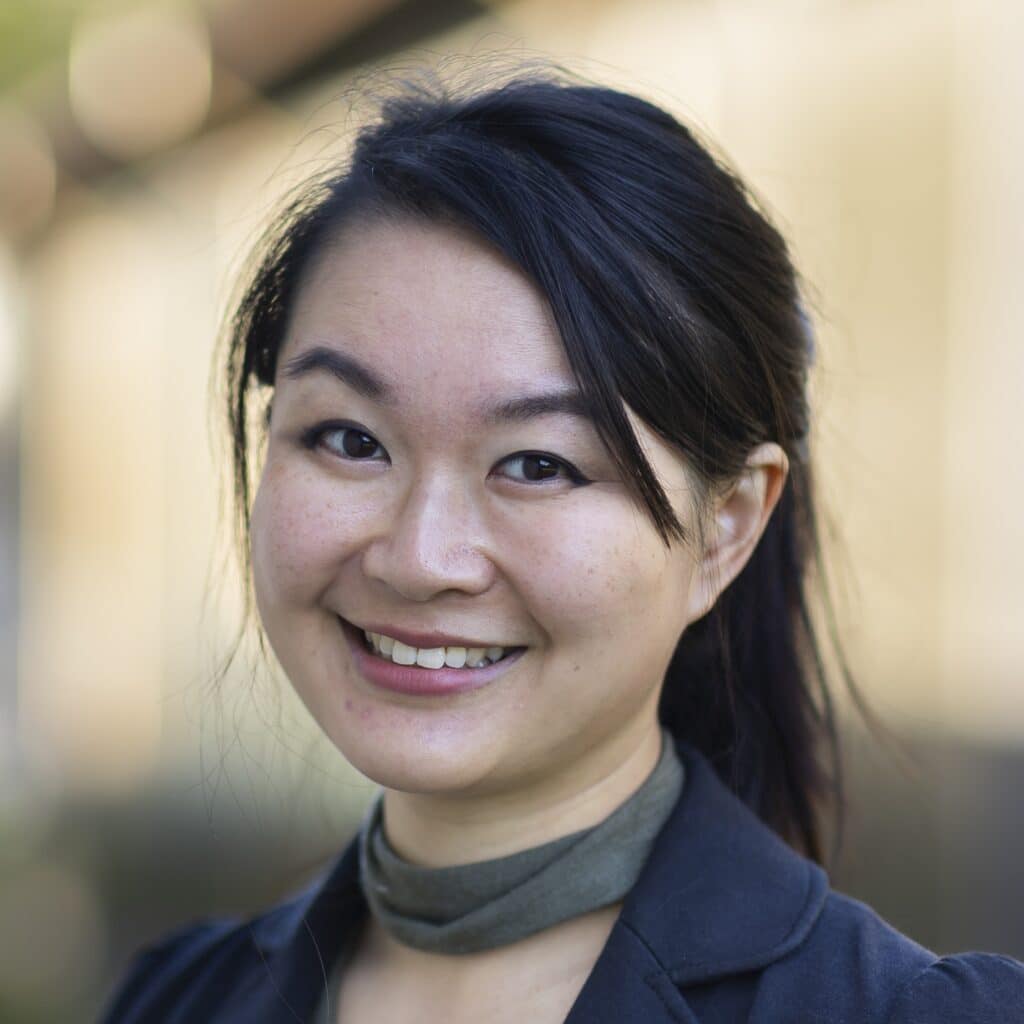
Dr Amy H Y Chan
Associate Professor, School of Pharmacy
The University of Auckland
Dr Amy H Y Chan
Dr Chan is an Associate Professor at The University of Auckland School of Pharmacy and co-lead of their Medicines intelligence group. She is a clinical pharmacist with over 15 years’ experience working in the public hospital sector, where she led one of the clinical pharmacy teams. Dr Chan has nearly 20 years’ clinical and research experience working in the public sector, and has particular interest in understanding how digital innovations can improve medicines use and health outcomes. She is currently involved in leading several large programmes of work relating to the evaluation of health interventions, use of big data and digital technology to improve healthcare delivery. Amy been involved in over 80 different health research projects and has influenced policy at a national and international level including global health guidelines and civil society policies. Amy also holds Minister-appointed positions on national boards and committees and provides consultancy to charities, medical research organisations, non-government organisations and global health organisations including WHO, FIP and CPA.
Digital tools for decentralized trials and digital endpoints
The availability of digital tools will completely revolutionise the conduct of clinical trials and future pharmacoepidemiology studies. Digital tools have allowed the creation of digital endpoints and the conduct of decentralised clinical trials (DCTs). These are poised to fundamentally reshape pharmacoepidemiology research and analysis and health research. By leveraging digital technologies—such as wearable sensors, mobile apps, and remote monitoring devices—researchers can now continuously collect high-quality, real-world data on patient outcomes directly from participants in their natural environments, rather than relying solely on clinic visits which are often episodic and infrequent. This shift enables a more authentic and granular understanding of how patients feel, function, and behave in their everyday lives, providing valuable insights into disease burden and treatment effects that previously were not visible nor accessible to researchers. For pharmacoepidemiologists, these innovations offer several key advantages. First, digital endpoints facilitate more efficient and accurate screening, earlier disease detection, and continuous monitoring, which can improve the sensitivity and relevance of outcome measures. The increased volume and diversity of data generated through DCTs also allow for more robust statistical analyses, supporting adaptive trial designs and more nuanced subgroup analyses. Decentralised approaches expand access to broader and more diverse populations, enhancing the generalizability of findings and reducing traditional barriers related to geography and clinic access. However, these advances also introduce new analytical challenges. The remote and continuous nature of data collection requires rigorous attention to data integrity, privacy, and management, as well as sophisticated statistical methods to handle missing data, variation in data quality, and potential biases introduced by remote participation. Regulatory frameworks are evolving to address these complexities. There is a need for interdisciplinary collaboration and robust infrastructure to ensure high-quality research that is responsive to the changing health needs of our populations. Digital endpoints and DCTs are the future for health research and will empower pharmacoepidemiologists to deliver more patient-centered, timely, and actionable evidence on medication safety and effectiveness. This presentation will discuss how these digital tools will help drive a paradigm shift toward real-world, data-driven insights to accelerate therapeutic innovation and improve health outcomes for all.

Dr Mary Beth Ritchey
Principal and Owner, Med Tech Epi;
ISPE Immediate Past-President
Dr Mary Beth Ritchey
Mary Beth Ritchey MSPH, PhD, FISPE has spent her career dedicated to better understanding medical product safety and effectiveness within the “real world” where patients are managing new and chronic health conditions in an increasingly complex health care system. She is an expert in leading multi-stakeholder international clinical research, strategic planning and coordination of scientific programming, development of actionable policies, and enabling rigorously accurate plain-language information to aid informed decisions about medical products.
Dr. Ritchey’s career has encompassed roles within industry, academia, and government – including as the former Chief Epidemiologist for devices at the US FDA. Currently, as Founder, Principal and Owner of Med Tech Epi, she provides innovative strategy and conducts rigorous evidence generation studies. Additionally, as part-time faculty in the Center for Pharmacoepidemiology and Treatment Science at Rutgers University, she teaches and mentors students. She has been active in the International Society for Pharmacoepidemiology (ISPE) throughout her career, chairing the ISPE Annual Meeting in 2016 and is the current Immediate Past President. Dr. Ritchey holds bachelor's degrees in chemistry (Duke University) and nursing (University of North Carolina [UNC] Chapel Hill) as well as Masters and Doctoral degrees in epidemiology from the UNC Gillings School of Global Public Health.
From Data to Decisions: How Real-World Evidence Transforms Healthcare Policy and Practice
Advances in real-world evidence (RWE) have dramatically expanded its influence on clinical guidelines, regulatory decisions, and health system policies worldwide. As the volume and rigor of RWE increase, translating these insights into tangible healthcare improvements remains a complex challenge—requiring not only scientific excellence but also effective collaboration and communication among diverse stakeholders.
Despite significant progress, persistent barriers remain. Converting nuanced, context-rich real-world data (RWD) into RWE which informs policies that are both responsive and sustainable often necessitates aligning competing priorities and demonstrating relevance in domains traditionally dominated by randomized controlled trials. The most compelling examples—where RWE has facilitated regulatory approvals, updated clinical guidelines, or influenced reimbursement decisions—highlight both the potential and complexity of translating RWD into real-world impact.
This presentation will illustrate how RWE has driven meaningful policy and practice changes, showcasing key case studies. Drawing on her leadership and experience, Dr. Ritchey will share practical strategies for overcoming translational barriers. She will emphasize the importance of stakeholder engagement, methodologic transparency, and ongoing dialogue between RWD holders, RWE generators, and decision-makers.
By reflecting on both successes and ongoing challenges, this session aims to equip RWE professionals with insights and strategies to accelerate the translation of data into improved patient outcomes and public health. Ultimately, it demonstrates how real-world research can be a powerful catalyst for sustained, meaningful change in generating actionable evidence for medical products.